Two New Studies Investigate The Significance Of Minimal Residual Disease In Multiple Myeloma
The results of two recent European studies provide new insights into minimal residual disease detection and its potential value in the treatment of multiple myeloma.
The first study, carried out in Spain, used two different methods to detect minimal residual disease (MRD) in myeloma patients. The study found that the two methods led to similar results, and that MRD levels may be a better predictor of patient prognosis than traditional measures of treatment response.
The second study was conducted by researchers in Britain using data from a large clinical trial carried out there. The researchers evaluated minimal residual disease in trial participants using a technique called multiparameter flow cytometry. This technique also was one of the two used in the Spanish study.
They British investigators found that MRD status predicted survival outcomes in myeloma patients who received an autologous (own) stem cell transplant.
In an editorial accompanying the British study, Dr. Nikhil Munshi and Dr. Kenneth Anderson, both from the Dana-Farber Cancer Institute in Boston, discuss the value of minimal residual disease in multiple myeloma. They write, "If validated in future studies, MRD may serve as a biomarker to inform therapy and as a surrogate for [overall survival]. Specifically, achieving MRD-negative status may become a goal of future studies using induction, transplantation, consolidation, and/or maintenance therapies."
They add, "With available technologies and ease of MRD measurement, it is now time to carry out additional large prospective studies to define the clinical significance of MRD and its impact on patient outcome in myeloma."
Background
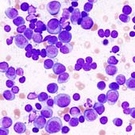
Tests to determine whether or not a myeloma patient has minimal residual disease are carried out using cells from a patient’s bone marrow.
The tests are typically conducted in cases where a patient has achieved a complete response based on urine and blood tests. The MRD tests are much more sensitive than urine and blood tests at detecting the presence of myeloma, and thus are a more accurate way of determining whether the patient has any remaining (residual) signs of disease.
Patients who have no signs of residual disease are described as being MRD-negative, while those with signs of residual disease in their marrow are categorized as MRD-positive.
According to Dr. Joaquin Martinez-Lopez from Hospital Universitario 12 de Octubre in Madrid, approximately 30 percent to 50 percent of myeloma patients reach a complete response with current treatments. “However, most of these patients continue to relapse due to persistence of minimal residual disease,” said Dr. Martinez-Lopez. “Therefore, more sensitive techniques are required to define response."
One established method for measuring MRD in myeloma patients is a technique called multiparameter flow cytometry. A newer method, evaluated by Dr. Martinez-Lopez and his colleagues in the Spanish study, is called genetic deep sequencing.
Researchers use gene sequencing to determine an individual patient's genetic information. They can study myeloma-related genetic mutations by comparing the sequence of normal cells and myeloma cells. In deep sequencing, particular genetic regions are sequenced multiple times.
Prognostic Value Of Deep Sequencing Method For MRD Detection
Dr. Martinez-Lopez reported results of the Spanish study at the ASCO 2013 Meeting held in Chicago earlier this month (abstract).
In this study, Dr. Martinez-Lopez and his colleagues sought to compare the prognostic value of traditional response criteria and MRD measurements using multiparameter flow cytometry and deep sequencing.
The researchers evaluated bone marrow samples from 68 multiple myeloma patients who had participated in two Spanish clinical trials. These samples were collected at diagnosis and after treatment.
They found that the MRD detection results obtained from the two methods were similar. According to both methods, 34 patients were MRD-positive and 9 were MRD-negative. Three additional patients were identified as MRD-negative by one of the methods but MRD-positive by the other.
Patients who were MRD-negative had significantly better median overall survival (not yet reached), compared to patients who were MRD-positive (86 months).
Among the patients who had reached a complete response, 24 patients were MRD-positive and 10 patients were MRD-negative. In this subgroup, the MRD-negative patients also maintained a better median overall survival (not yet reached) compared to the MRD-positive patients (81 months).
Dr. Martinez-Lopez concluded that the study's findings “may contribute to the design of patient-specific treatment approaches, such as de-escalation of therapy for MRD-negative patients or escalation of treatment for MRD-positive patients."
MRD Status And Survival Outcomes
In a second study, British researchers investigated the prognostic value of MRD assessment in myeloma patients who participated in a large, multi-center Phase 3 trial -- the so-called MRC Myeloma IX trial.
Patients in this study were divided into two groups based on whether they received intensive or non-intensive therapy.
Those in the intensive-pathway treatment group received induction therapy with either cyclophosphamide (Cytoxan), thalidomide (Thalomid), and dexamethasone (Decadron) or cyclophosphamide, vincristine (Oncovin), doxorubicin (Adriamycin), and dexamethasone, followed by high-dose melphalan (Alkeran) and an autologous stem cell transplant.
Patients in the non-intensive pathway group either received induction therapy with melphalan and prednisone or a combination of cyclophosphamide, thalidomide, and dexamethasone.
After treatment, patients in both groups were randomly assigned to receive thalidomide-based maintenance therapy or no further therapy.
Researchers assessed MRD in 378 intensive-pathway patients after induction therapy, 397 intensive-pathway patients 100 days after transplantation, and 245 non-intensive pathway patients after induction therapy.
They found that MRD-negative status was associated with significantly better outcomes in intensive-pathway patients. The median progression-free survival for MRD-negative patients after stem cell transplantation was 28.6 months from the date of MRD assessment, compared to 15.5 months for patients who were MRD-positive after transplantation.
Furthermore, the median overall survival in MRD-negative patients after transplantation was 80.6 months from the date of MRD assessment, versus 59 months in MRD-positive patients after transplantation.
Outcomes between MRD-negative and MRD-positive patients in the non-intensive pathway group were similar. The median progression-free survival at the end of induction therapy was 10.5 months for MRD-negative patients and 7.4 months for MRD-positive patients.
The researchers also evaluated the impact of thalidomide-based maintenance therapy in both groups of patients. Patients who were MRD-negative and received thalidomide maintenance therapy had the longest progression-free survival, while those who were MRD-positive and receiving no maintenance therapy had the shortest progression-free survival (approximately 39 months versus 12 months, from time of MRD assessment).
Notably, 28 percent of MRD-positive patients who received thalidomide maintenance therapy became MRD-negative, compared to 3 percent of MRD-positive patients who received no further therapy.
However, the researchers found that thalidomide maintenance therapy did not significantly improve progression-free survival of patients who were already MRD-negative prior to maintenance therapy.
Based on their results, the researchers suggest that a thalidomide-based maintenance regimen may eliminate MRD in some patients.
In response to the results of the British study, Dr. Munshi and Dr. Anderson wrote that the study “confirms the feasibility of carrying out MRD analysis in a large majority of patients enrolled in a multi-center study and demonstrates the clinical utility of this assay.”
For more information on the British study (abstract) and the editorial (full text, PDF) written by Drs. Munshi and Anderson, please see the Journal of Clinical Oncology.
Related Articles:
- None Found

