Extramedullary Disease Presents Unique Symptoms And Challenges In Multiple Myeloma Patients
A recent Greek study highlights the distinct symptoms and disease course of multiple myeloma patients who develop extramedullary disease at relapse.
The results are consistent with those from previous studies and demonstrate that myeloma patients who develop extramedullary disease have poorer overall survival than those who do not. Furthermore, the study investigators identified clinical differences at diagnosis and at relapse between myeloma patients with and without extramedullary disease.
They conclude that myeloma patients with extramedullary disease exhibit a particularly aggressive and treatment-resistant form of myeloma, posing unique therapeutic challenges.
Background And Patient Population
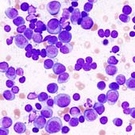
Extramedullary disease occurs when myeloma cells form tumors outside of the bone marrow, in the soft tissues or organs of the body. The true prevalence of extramedullary disease in multiple myeloma patients has yet to be determined; prior studies have reported rates ranging from 7 percent to 15 percent in newly diagnosed myeloma patients and from 6 percent to 20 percent in relapsed patients.
Previous research has shown that myeloma patients with extramedullary disease have a poorer prognosis than those without. However, the mechanisms underlying extramedullary disease are still not well understood.
In the current study, Greek researchers sought to observe the frequency of extramedullary disease in myeloma patients, along with their symptoms, laboratory measurements, and survival outcomes.
They retrospectively evaluated data from 303 multiple myeloma patients who were treated between 1998 and 2011. Of these patients, 9 percent eventually developed extramedullary disease.
Clinical Features Of Extramedullary Disease
Extramedullary disease at relapse was most commonly found in the liver (25 percent), lungs (21 percent), lymph nodes (17 percent), and mouth (13 percent).
Myeloma patients who developed extramedullary disease demonstrated a different set of symptoms, both at the time of initial diagnosis and at relapse, than those who did not. At the time of initial myeloma diagnosis, patients who eventually developed extramedullary disease had higher rates of elevated levels of lactate dehydrogenase (LDH) in the blood (38 percent versus 18 percent), bone tumors (57 percent versus 27 percent), and bone fractures (35 percent versus 11 percent).
At the time extramedullary disease was detected, 28 percent of patients with extramedullary disease had experienced weight loss and disease-related fever, which are rare in multiple myeloma patients without extramedullary disease. In addition, 93 percent of patients with extramedullary disease demonstrated elevated serum LDH levels, and the median level of paraprotein in the blood at extramedullary relapse was less than half of what it was at diagnosis.
Treatment Before And After Extramedullary Disease
Patients who developed extramedullary disease had been treated with a median of three regimens prior to developing extramedullary disease. These regimens included high-dose chemotherapy and stem cell transplantation (32 percent), thalidomide (Thalomid) (50 percent), Velcade (bortezomib) (50 percent), and Revlimid (lenalidomide) (46 percent). Myeloma patients in the Greek study who did not develop extramedullary disease had also been treated with a median of three prior treatments, including stem cell transplantation (24 percent), thalidomide (40 percent), Velcade (67 percent), and Revlimid (23 percent).
Due to the retrospective nature of the study, the researchers were hesitant to draw conclusions regarding the relationships between prior treatment regimens and extramedullary disease at relapse.
Their analysis showed, however, that use of high-dose chemotherapy plus stem cell transplantation, as well as treatment with thalidomide and Revlimid, were not significantly different between those who did and those who did not develop extramedullary disease. This is worth noting since stem cell transplantation, thalidomide, and Revlimid have been considered potential risk factors for extramedullary disease. The investigators did find, though, that patients previously treated with Velcade had a lower risk of developing extramedullary disease.
After the onset of extramedullary disease, patients were treated with Velcade-based regimens (32 percent), platinum-containing regimens (21 percent), Revlimid (21 percent), as well as vincristine (Oncovin) plus doxorubicin (Adriamycin) and dexamethasone (Decadron) (8 percent).
Notably, most cases of extramedullary disease occurred in more recent years, between 2007 and 2011. This finding is comparable to those of earlier studies, which have reported a higher frequency of extramedullary disease in the era of novel agents (see related Beacon news).
Survival Results
The median overall survival after extramedullary relapse was five months.
From the time of their initial myeloma diagnosis, the median overall survival for patients who developed extramedullary disease was 38 months, compared to 59 months for patients who did not develop extramedullary disease. These results are in line with those of previous studies investigating survival outcomes for myeloma patients with and without extramedullary disease (see related Beacon news).
Discussion
In the discussion of their results, one topic the study investigators address is the fact that, as mentioned earlier, most of the cases of extramedullary relapse in their sample of patients were detected in the last four years of their data.
The investigators suggest that extramedullary disease may be more easily detected in recent years due to better imaging and diagnostic tests as well as better physician awareness.
In a commentary accompanying the study, Dr. Philippe Moreau from the University of Nantes in France and Dr. Aaron Polliack from Hadassah University Hospital in Jerusalem, who were not involved in the study, state that as novel agents extend the survival of myeloma patients, extramedullary disease may become more prevalent.
Since patients who later developed extramedullary disease were more likely to have had high LDH, bone tumors, and bone fractures at diagnosis, the study investigators state these findings support the theory that certain myeloma patients have more aggressive disease from the onset.
Dr. Moreau and Dr. Polliack note in their commentary that while this and several previous studies have reported a poor prognosis for myeloma patients with extramedullary disease, all of these studies are limited by their retrospective nature and small patient population. Without larger, prospective studies, they warn that it is difficult to estimate the true frequency of extramedullary disease and determine the best therapeutic options.
Dr. Moreau and Dr. Polliack also raise additional questions to address in the future: Are extramedullary relapses more frequent in the era of novel agents, and if so, why? Will patients with extramedullary relapse benefit from combination therapies, and, if so, which combinations would be appropriate and more effective?
For more information, please see the study (abstract) and commentary (subscription required) in the journal Leukemia and Lymphoma.
Related Articles:
- None Found

I found it interesting that extra medullary disease is often associated with an increased level of lactase dehydrogenase (LDH). The blood test for LDH is routinely done for my myeloma , and I think that it is usually done at the time of diagnosis. LDH testing is done for other blood cancers too. What is the connection between LDH and extramedullary disease? Is it that there is a higher rate of cell lysis (destruction) in patients with elevated LDH, and if so, how is that connected?
When my husband was diagnosed, he had both extramedullary and in-marrow myeloma. When he relapsed 8 months after his stem cell transplant, though, there didn't seem to be any marrow activity (m-spike still at 0.0, PET scan only showing activity at the lumps). I can't seem to find any info on whether he still falls in the category they're discussing here (aggressive myeloma), or if they are only referring to people whose bone marrow becomes actively involved again. I'm wondering if there is any info in this report, or elsewhere, that discusses the progression of extramedullary without marrow involvement...is it the same, better, worse? I'd appreciate any info, if people have seen this discussed elsewhere! Thanks!
Emily,
My husband developed extramedullary 5 months after his initial MM diagnosis. He had a M-spike of 5.0 when he was orginially diagnosed and staged at 3A. With treatment of Velcade/Dex/Revlimid it dropped to < .5 and the PET looked good, but then EM developed.
After his SCT his M-spike stayed low and the bone tumors were gone, but the extramedullary tumors redeveloped just 53 days after transplant and the newly released Kyprolis® (carfilzomib) had no impact. At the time of his death (5 months after the SCT) the bone tumors had also returned. It had been several weeks since his last M-spike so I don't know what it was.
Progress toward fundraising goal
for all of 2020:
15%
For more information, see the Beacon's
"2020 Fundraising: Goals And Updates" page