Long-Term Analysis Highlights Potential Survival Benefit Of Auto-Allo Transplantation In Multiple Myeloma
By: Virginia Li; Published: March 27, 2013 @ 6:48 pm | Comments Disabled
Long-term results from a European study indicate that an autologous stem cell transplant followed by a reduced-intensity donor transplant may lead to better survival outcomes in multiple myeloma patients than either a single autologous transplant or two back-to-back autologous transplants.
After a median follow-up of eight years, patients who received an autologous stem cell transplant followed by a reduced-intensity donor (allogeneic) stem cell transplant had higher progression-free and overall survival rates than patients who received either a single autologous transplant or two back-to-back autologous transplants.
An important caveat to these results is that the European study was started at a time when treatment with novel myeloma agents, such as thalidomide [1] (Thalomid), Velcade [2] (bortezomib), or Revlimid [3] (lenalidomide), was not yet common.
Since the introduction of novel agents, the life expectancy of multiple myeloma patients has significantly improved. This, in turn, has raised questions about the appropriate role of stem cell transplantation in the treatment of myeloma.
In addition, some recent studies, which have included treatment with novel agents, have suggested that back-to-back ("tandem") autologous and reduced-intensity allogeneic stem cell transplants may not offer a survival benefit compared to tandem autologous transplants.
The authors of the European study, however, believe the more recent studies may not have had long enough follow-up times to adequately compare the two transplant regimens.
Thus, the study investigators believe tandem autologous/reduced-intensity allogeneic transplantation is a treatment option that deserves further consideration — particularly for younger myeloma patients with high-risk disease.
The new study is an update to a previous analysis published in 2011 (see related Beacon [4] news).
Background
Despite recent advances in the treatment of multiple myeloma, the disease continues to be incurable for the majority of patients.
Donor stem cell transplantation, however, has the potential to be a curative therapy for myeloma.
In this procedure, a patient is first treated with a "conditioning" regimen, consisting of radiation and/or chemotherapy, which kills off many of the patient's myeloma cells. The conditioning regimen, however, also kills off many of the patient's healthy stem cells.
Thus, after the conditioning regimen, the patient is given stem cells from a healthy donor.
The transplanted stem cells replenish those lost during the pre-transplant conditioning regimen.
In addition, the transplanted cells may also attack, or keep at bay, any remaining myeloma cells in the transplant recipient's body, a process known as the "graft-versus-myeloma" effect. If the graft-versus-myeloma effect is completely successful, the transplant is curative.
The downside to donor stem cell transplantation is that can involve serious complications.
For example, the donor cells may attack the healthy cells of the transplant recipient, resulting in what is known as graft-versus-host disease (GVHD).
GVHD and other serious risks associated with donor stem cell transplantation are the reason why the treatment remains controversial, despite its curative potential (see related Beacon [5] news).
Study Design
In the current study, European researchers compared survival outcomes between myeloma patients who received tandem autologous/reduced-intensity conditioning allogeneic ("auto-RICallo") transplants with those who received either a single autologous transplant or tandem autologous transplants.
Between February 2001 and January 2005, the researchers recruited 357 multiple myeloma patients under the age of 70 years who were in stable disease or better after their initial anti-myeloma treatment.
Patients were divided into two treatment groups; 108 patients with available sibling donors were assigned to the tandem auto-RICallo transplant group, and 249 patients were assigned to the autologous transplant group.
Those in the autologous transplant group had the option to undergo either a single transplant or tandem autologous transplants.
Approximately a quarter of patients in both the tandem auto-RICallo group and the autologous transplant group had the del(13) chromosomal abnormality. The researchers mention that, although del(13) itself is not a strong predictor of treatment outcomes, it was at the time the only chromosomal abnormality that could be adequately analyzed at all treatment centers participating in the study.
Moreover, the authors note that patients who have the del(13) abnormality also often have other chromosomal abnormalities – such as del(17p), t(14;16), or t(14;20) – which recently have been linked to poor treatment outcomes.
Prior to entering the study, patients in both the transplant groups received initial treatment with a combination of vinicristine [6] (Oncovin), doxorubicin [7] (Adriamycin), and dexamethasone [8] (Decadron) (VAD) or other similar regimens. No patients in the study had initial treatment that included a novel agent.
The autologous stem cell transplants during the study were preceded by a conditioning (pre-transplant) regimen involving a standard dose of 200 mg/m2 of melphalan [9] (Alkeran).
The allogeneic transplants during the study were preceded by a reduced-intensity conditioning regimen that is not as destructive of stem cells as high-intensity ("myeloablative") regimens such as the standard dose of melphalan.
Reduced-intensity conditioning is often used prior to donor transplants to lower the risk of severe transplant-related side effects. Such transplants are also sometimes called "mini," or "non-myeloablative," allogeneic transplants.
The reduced-intensity conditioning regimen consisted of 30 mg/m2 of fludarabine (Fludara) for three days plus low-dose total body irradiation.
Patients in the study could choose, of course, to undergo further treatment if their disease eventually progressed.
Thus, most of the patients from both treatment groups also eventually received a variety of other treatments, including additional transplants (autologous or donor) and treatment with older as well as novel anti-myeloma agents.
In addition, twenty percent of the patients in the tandem auto-RICallo transplant group received donor lymphocyte infusions, a process in which white blood cells are collected from the stem cell donor and infused into the myeloma patient.
Survival Outcomes
Patients who received tandem auto-RICallo transplants as part of the original study design had better survival outcomes than those who received either single or tandem autologous transplants.
The progression-free survival rates at 8 years after first transplant were 22 percent and 12 percent for the two groups, respectively.
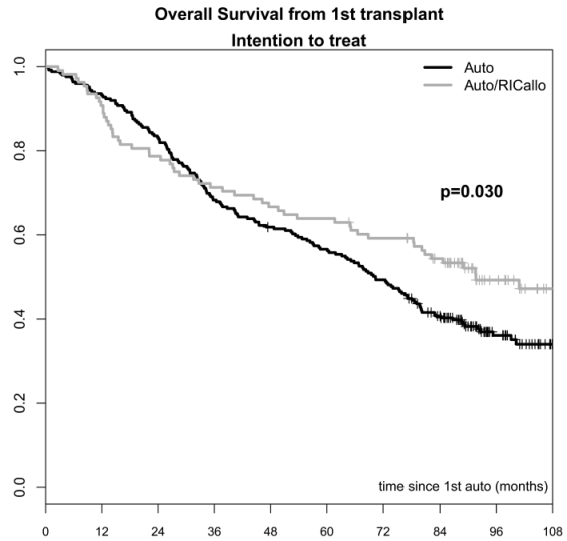
In addition, the overall survival rates at 8 years were 49 percent and 36 percent, respectively (see figure on the right).
The overall survival advantage for the tandem auto-RICallo regimen began to appear about 2 to 3 years after patients received their first transplant.
Prior to that point, complications related to donor transplantation caused overall survival to be lower in the patients who received tandem auto-RICallo transplants versus those who had either single or tandem auto transplants.
A fair question that could be asked is whether the survival advantage seen for the auto-RICallo regimen is due to the fact that some of the patients in the comparison (autologous transplant) group received only a single transplant.
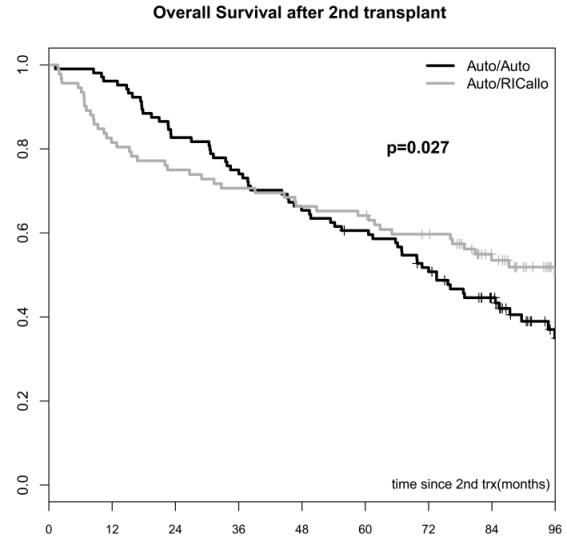
The survival advantage for the auto-RICallo regimen persists, however, when comparisons are made only for patients who, as part of the study design, received two transplants.
The overall survival rate at 8 years after second transplant was 52 percent for the auto-RICallo patients, and 35 percent for patients who had tandem autologous transplants (see figure on the right).
The auto-RICallo regimen also performed better in patients with the del(13) chromosomal abnormality.
Among these patients, the eight-year overall survival rate was 47 percent for patients who received tandem auto-RICallo transplants, compared to 31 percent for patients who received only single or tandem autologous transplants.
In comparison, among patients without the del(13) abnormality, eight-year overall survival was 55 percent and 46, respectively.
Based on these findings, the researchers suggest that donor transplants may partially overcome poor outcomes predicted by chromosomal abnormalities such as del(13) (see related Beacon [12] news).
Safety Outcomes
Among patients who received tandem auto-RICallo transplants, 31 percent experienced acute graft-versus-host disease (GVHD), which occurs within the first 100 days after a transplant, and 54 percent developed chronic GVHD, which occurs more than 100 days after a transplant.
Overall, the treatment-related death rate was 13 percent in the auto-RICallo patient group. In comparison, patients who had tandem auto-auto transplants as part of the study design experienced a treatment-related death rate of only 3 percent.
Most of the treatment-related deaths in the auto-RICallo group occurred among patients who experienced acute GVHD. The treatment-related death rate in that group of patients was 36 percent, compared to 4 percent in patients who did not experience acute GVHD.
Discussion
Two studies similar to the current one have been conducted in recent years.
In one prior study (abstract [13]; Beacon [14] review of related conference presentation), progression-free survival and overall survival for patients undergoing tandem auto-RICallo transplants did not differ significantly from the survival rates seen in tandem autologous transplant patients.
However, the authors of the current study point out that survival outcomes in this first study were measured after a median follow-up of only three years. The investigators believe that a follow-up of at least five years is needed to properly assess the value of tandem auto-RICallo transplantation in myeloma patients.
In a second study (full text [15]), tandem auto-RICallo transplantation did not provide a significant survival advantage versus auto transplantation followed by maintenance therapy.
However, in that study, the tandem auto-RICallo patients received only low-dose total body radiation as conditioning prior to their donor transplant. They did not receive any fludarabine.
In addition, the authors of the current study note that, even though there was no difference in overall survival between the two patient groups in the second study, the relapse/progression rate at six years in that study was noticeably lower in the auto-RICallo patients than in the patients who received only an autologous transplant (55 percent versus 79 percent, respectively).
Thus, the authors believe tandem auto-RICallo transplantation still deserves further investigation as a potential treatment option for myeloma patients.
In particular, they believe it may be well suited to younger patients with higher-risk disease. The results of the current study suggest that tandem auto-RICallo transplants seem to be beneficial to patients with high-risk disease, and younger patients who receive donor transplants generally experience lower treatment-related death rates than older patients.
For more information about the current study, please see the article in the journal Blood [16] (abstract).
Article printed from The Myeloma Beacon: https://myelomabeacon.org
URL to article: https://myelomabeacon.org/news/2013/03/27/long-term-analysis-autologous-allogeneic-transplantation-survival-outcomes/
URLs in this post:
[1] thalidomide: https://myelomabeacon.org/resources/2008/10/15/thalidomide/
[2] Velcade: https://myelomabeacon.org/resources/2008/10/15/velcade/
[3] Revlimid: https://myelomabeacon.org/resources/2008/10/15/revlimid/
[4] Beacon: https://myelomabeacon.org/news/2011/08/26/mini-donor-stem-cell-transplant-as-second-transplant-may-improve-outcomes-in-multiple-myeloma/
[5] Beacon: https://myelomabeacon.org/news/2010/09/13/experts-recommend-against-donor-stem-cell-transplantation-for-multiple-myeloma-patients-until-safety-and-efficacy-is-improved/
[6] vinicristine: https://myelomabeacon.org/resources/2008/10/15/vincristine/
[7] doxorubicin: https://myelomabeacon.org/resources/2008/10/15/doxorubicin/
[8] dexamethasone: https://myelomabeacon.org/resources/2008/10/15/dexamethasone/
[9] melphalan: https://myelomabeacon.org/resources/2008/10/15/melphalan/
[10] Image: http://static9.light-kr.com/images/original/research/GahrtonEtAl-OS-Auto-vs-Auto-RICAllo.png
[11] Image: http://static9.light-kr.com/images/original/research/GahrtonEtAl-OS-Auto-Auto-vs-Auto-RICAllo.png
[12] Beacon: https://myelomabeacon.org/news/2013/02/06/tandem-auto-allo-transplantation-prognosis-of-high-risk-myeloma-patients/
[13] abstract: http://www.ncbi.nlm.nih.gov/pubmed/21962393
[14] Beacon: https://myelomabeacon.org/news/2010/12/06/donor-stem-cell-transplants-come-up-short-as-second-transplant-option-in-multiple-myeloma-patients-ash-2010/
[15] full text: http://bloodjournal.hematologylibrary.org/content/119/26/6219.long
[16] Blood: http://bloodjournal.hematologylibrary.org/content/early/2013/03/12/blood-2012-11-469452.abstract
Click here to print.