Itraconazole May Worsen Velcade-Induced Side Effects In Relapsed Multiple Myeloma Patients
A small study in Japan showed that relapsed multiple myeloma patients treated simultaneously with Velcade and itraconazole experienced greater Velcade-induced side effects, such as lower platelet levels and nerve damage to the extremities, than patients who did not receive itraconazole.
The researchers recommended that multiple myeloma patients receiving both Velcade (bortezomib) and itraconazole (Sporanox) be closely monitored for Velcade-induced side effects throughout the duration of their treatment.
However, according to Dr. Paul Richardson of the Dana-Farber Cancer Institute in Boston the results of the study should be interpreted cautiously. “Patients from Japan can have unique toxicities,” he explained in an email to The Myeloma Beacon.
Itraconazole is used for the treatment of fungal infections. These infections most often begin in the lungs and may spread through the body. In addition to treating fungal infections in the lungs, itraconazole is also used to treat infections of the fingernails and toenails and yeast infections of the mouth and throat.
Fungal infections can occur in multiple myeloma patients. According to Dr. Craig Hofmeister of the Ohio State University Medical Center, however, fungal infections are “rare except for patients given higher doses of dexamethasone that have an increased risk of oral thrush (oral candida). Invasive fungal infections are rare.”
Both Dr. Richardson and Dr. Hofmeister indicated to The Myeloma Beacon that they currently do not use itraconazole for the treatment of fungal infections.
Itraconazole works by inhibiting an enzyme needed for fungi to grow properly. However, it also inhibits liver enzymes responsible for breaking down Velcade for excretion.
The inhibition of these enzymes can cause Velcade to accumulate in the body, resulting in an increase in the severity of its side effects. This study sought to determine if the co-administration of itraconazole with Velcade worsened Velcade-induced side effects in relapsed myeloma patients.
Six Japanese patients were included in the study. All six patients received intravenous Velcade and oral dexamethasone (Decadron) as part of a 21-day treatment cycle. Half of the patients also received itraconazole in addition to Velcade and dexamethasone.
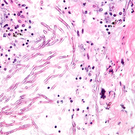
Only the patients who received both Velcade and itraconazole experienced worsened nerve damage to the extremities (peripheral neuropathy). Velcade treatment was stopped for two of these patients, which was followed by an improvement in the damage.
All three patients who received both Velcade and itraconazole had severely low platelet levels (thrombocytopenia). They needed platelet transfusions before they could continue therapy. The patients who did not receive itraconazole did not experience as severe a loss of blood platelets.
The effect of other antifungal medications on Velcade-induced side effects has been investigated in at least two American studies.
One study investigated the use of ketoconazole (Nizoral) with Velcade in patients with solid tumors. Another study determined the side effects resulting from co-administration of omeprazole (Losec) with Velcade in patients with a variety of cancers, including multiple myeloma. Although these medications all treat fungal infections, they each inhibit different enzymes involved in the breakdown of Velcade.
Researchers in the first study found that ketoconazole slowed the clearance of Velcade from the liver. This resulted in a 35 percent increase in exposure to Velcade for patients who received both drugs.
Unlike the Japanese study, however, neither study found that the antifungals increased the severity of Velcade-induced side effects.
“It would be ideal if a group, such as Mayo Clinic, that has a clinical database with concomitant medications could analyze for an association between peripheral neuropathy, thrombocytopenia, and itraconazole or other medications interacting with [the enzyme] CYP3A4,” said Dr. Hofmeister.
For more information, please see the Pharmacotherapy (abstract).
Related Articles:
- None Found
